Impact of Prone Transpsoas Fusion on Sagittal Alignment and Reduction of Isthmic Spondylolisthesis
Ergin Coskun, MD
Isaac Moss, MDCM, MASc, FRCSC
Patient History and Examination
The patient is a 58-year-old female who presented with a longhistory of severe lower back pain and radicular symptoms. The complained of constant painful pressure in her low back that worsens with extension. Her radicular symptoms were in the nerve distribution, right side symptoms worse than left.
She had 4 out of 5 right ankle dorsiflexion, the remainder of her lower extremity motor exam was intact. She ambulatedwith a forward flexed posture and an antalgic gait. Despite extensive conservative treatment, her symptoms persisted resulting in severe disability.
Pre-operative Imaging:
Lumbar x-rays revealed disc space collapse between L4 and L5, as well as a grade 2 lytic anterolisthesis at that levelresulting in severe neuroforaminal stenosis(Figure 1a-b) and mobility in flexion and extension views(figure 1c-d).
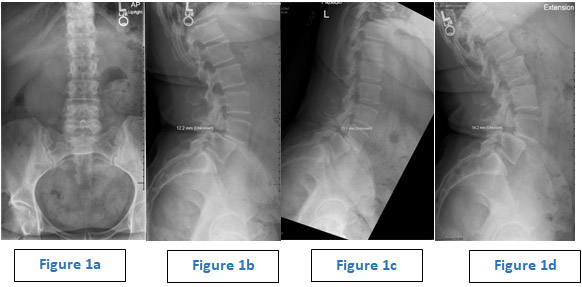
Sagittaland axial (figure2a-d) MRI images showed a relatively high-grade spondylolisthesis at L4-L5, resulting in severe neuroforaminal stenosis, and a synovial cyst of the facet joint at L3-L4, resulting in lateral recess stenosis (figure 2e).

Diagnosis:
According to her history, examination findings, and radiography results,she was suffering from lumbar radiculopathy due to spondylolisthesis and synovial cyst of facet joint.
Treatment:
Goals:L3-L4 decompression, L4-L5 decompression and posterior fusion to correct deformity and relieve the stenosis with minimal invasive technique.
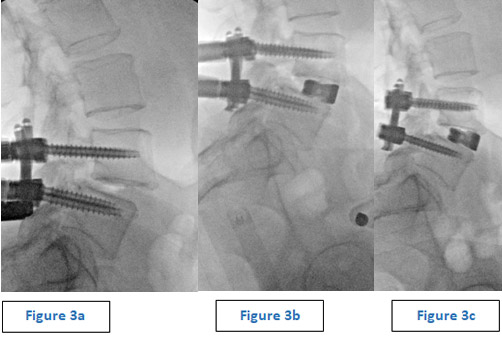
Selected surgical option: The surgical technique chosen was minimally invasive right-side laminectomy, medial facetectomy, synovial cyst removal at L3-L4andminimally invasive posterior percutaneouspedicle screw placement with preliminary reduction of the listhesis,followed by lateral lumbar interbody fusion via prone transpsoas approach at L4-L5 level ,relying on indirect decompression to relieve the neuroforaminal stenosis.
Significant slip reduction was achieved with posterior instrumentation (figure 3a). To do so, after screws were placed and the rods were passed, the L5 set caps were “final tightened” to lock the polyaxial tulips with the rod unreduced in the L4 tulips. Set cpas in the L4 extended screws tabs were then used to reduced L4 to the rods. The interbody fusion was then performed in the prone position via a transpsoas approach. After the interbody device had been placed, there was a small residual listhesis. Further reduction was then carried out by advancing the L4 screws and repeating the the reduction maneuver described above (figure 3c).
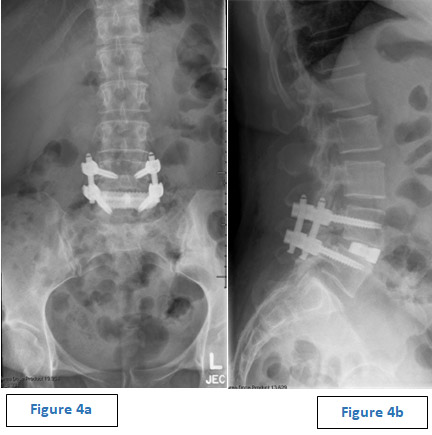
Outcome:
The patient tolerated the surgery well with <100cc of blood loss and no intraoperative complications.Postoperative images demonstrated appropriate restoration of sagittal alignment (320 of segmental lordosis) and a complete correction of the preoperative listhesis (figure 4a-b). The patient noted immediate improvement of her baselineback pain and radicular symptoms and was discharged homeon postoperative day 1.
Discussion:
Surgical intervention is generally recommended after conservative treatment fails in patients with spondylolisthesisin order to decompress the involved neural structures and prevent progression of the deformity.Surgical managementof the slipped vertebra may or may not involve reduction prior to fusion.The role of reduction remains debatable due to the associated risks which include neurologic deficits, prolonged operative time, and loss of reduction1.
Recent studies have demonstrated that reduction of lumbar spondylolisthesis is critical for optimizing fusion rate and reestablishing sagittal alignment by increasing the total endplate surface area available for interbody fusion between affected adjacent vertebrae1,2.Reduction of spondylolisthesis has not been shown to increase complication rates, thus it can be considered a safe surgical procedure2.
Lateral lumbar interbody fusion (LLIF), is a revolutionary technique for accessing the intervertebral disk via the retroperitoneal spaceused for the treatment of lumbar spondylolisthesis. The lateral decubitus position is the traditional method for performing this procedure3.Lateral positioning has the advantage of angling the patient to open the disc space aloowing for easier access and instrumentation4,5.In contrast, lateral positioning frequently necessitates patient repositioning in order to perform a concurrent posterior fusion. Additionally, lateral positioning is not ideal for restoration ofsagittal plane alignment.
The prone transpsoas (PTP) approach has been developed to overcome some of the LLIF’s issues 6,7. The PTP approach allows circumferential access to the lumbar spinefor indirect decompression, cage insertion, and subsequent posterior fusion without the requirement for patient repositioning.
There are some risks associated with theprone transpsoas LLIF technique, including transpsoas muscle swelling, hip flexor weakness, genitofemoral nerve irritation, and lumbar plexus/nerve root injury8.However, despite these risk inherent to tranpsoas surgery, we believethis techniqueis a powerful option to address higher-grade spondylolisthesis using minimally invasive principles with the ability ot access the anterior and posterior column simultaneously in a single position.
References:
Longo UG, Loppini M, Romeo G, Maffulli N, Denaro V. Evidence-based surgical management of spondylolisthesis: Reduction or arthrodesis in situ. Journal of Bone and Joint Surgery – Series A. 2014;96(1):53-58. doi:10.2106/JBJS.L.01012
- Lambrechts MJ, Barber JA, Beckett N, et al. Surgical Reduction of Spondylolisthesis during Lumbar Fusion: Are Complications Associated with Slip Correction? Clinical Spine Surgery. Published online 2021. doi:10.1097/BSD.0000000000001230
- Godzik J, Ohiorhenuan IE, Xu DS, et al. Single-position prone lateral approach: cadaveric feasibility study and early clinical experience. doi:10.3171/2020.6.FOCUS20359
- Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. Journal of Spine Surgery. 2015;1(1):2. doi:10.3978/J.ISSN.2414-469X.2015.10.05
- Lang G, Navarro-Ramirez R, Gandevia L, neurosurgery IH-W, 2017 undefined. Elimination of subsidence with 26-mm-wide cages in extreme lateral interbody fusion. Elsevier. Accessed September 26, 2021. https://www.sciencedirect.com/science/article/pii/S1878875017307234
- Pimenta L, Pokorny G, Amaral R, et al. Single-Position Prone Transpsoas Lateral Interbody Fusion Including L4L5: Early Postoperative Outcomes. World Neurosurgery. 2021;149:e664-e668. doi:10.1016/J.WNEU.2021.01.118
- Ozgur B, Aryan H, Pimenta L, Journal WT-TS, 2006 undefined. Extreme Lateral Interbody Fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Elsevier. Accessed September 21, 2021. https://www.sciencedirect.com/science/article/pii/S1529943005008703
- Sclafani JA, Kim CW. Complications associated with the initial learning curve of minimally invasive spine surgery: A systematic review. Clinical Orthopaedics and Related Research. 2014;472(6):1711-1717. doi:10.1007/S11999-014-3495-Z